Home healthcare: The next frontier
As India faces rising chronic diseases, an ageing population, and growing demand for continuity of care, home healthcare is rapidly shifting from a peripheral service to a strategic extension of hospital care.
As India navigates a rising chronic disease burden, an ageing population, and growing demand for continuity of care, hospitals are confronting the limits of infrastructure-dependent, facility-centric healthcare. A silent but powerful shift is underway—one that is moving care from hospital beds to patient bedrooms, from overcrowded OPDs to digital platforms, and from episodic visits to continuous monitoring. Home healthcare, once considered an add-on service, is rapidly becoming an inseprable component of the country’s healthcare transformation.
Vishal Lathwal, CEO, Apollo Home Healthcare says, “India’s healthcare system is at a crucial juncture with noncommunicable diseases accounting for >60 per cent of the entire burden & elderly population is projected to cross 190 million in the next 10 years. Therefore, the next phase of healthcare expansion will not only be driven by hospital expansion but also at home – where care can be delivered.”
Why home healthcare now?
The strongest justification for home healthcare comes from clinical outcomes. Across hospitals, experts agree that the model works best for post-operative patients, elderly individuals, and those with chronic conditions such as COPD, heart failure, diabetes and hypertension.
Dr (Prof) Ranjan Shetty, Lead Consultant – Cardiologist, Infantry Road, Medical Director – SPARSH Group of Hospitals points out that home Healthcare is best for those patients who are recovering from surgery, elderly individuals who face the challenge related to mobility, some chronic illness problems such as COPD, heart failure, diabetes, dementia, stroke rehabilitation, and individuals who require care related to wound, palliative support or physiotherapy as well.
He notes that providing well-structured care at home reduces exposure to infections a patient acquires from hospitals, improve comfort related to emotions and helps stabilise chronic conditions as well.
Echoing this, Dr Sanjeev Gupta, Medical Director, Sri Balaji Action Medical Institute and Action Cancer Hospital, Delhi shares, “Research also shows that care which is provided to patients in familiar surroundings reduces the chanced of infections acquired from hospitals, improve the psychological comfort and support the quick recovery.”
Patients recover better at home because they are mentally and physically more at ease.
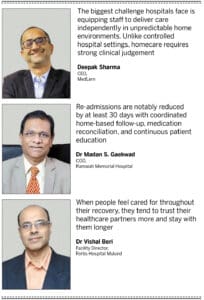
Dr Madan S. Gaekwad, COO, Ramaiah Memorial Hospital adds a deeper clinical view and adds, “Re-admissions are notably reduced by at least 30 days with coordinated home-based follow-up, medication reconciliation, and continuous patient education.” He emphasises that home settings allow clinicians to better assess environmental triggers, mobility challenges, and lifestyle gaps that impact recovery.
Homecare’s impact goes beyond clinical metrics. Family support becomes an active part of recovery, improving treatment adherence.
As Dr Vishal Beri, Facility Director, Fortis Hospital Mulund explains, “Family involvement in care planning increases medication adherence by 22 per cent and reduces readmissions by 20 per cent.”

The operational challenge: Hospitals know it works but can they deliver?
Even as clinical outcomes strongly favour homecare, hospitals face challenges integrating it into their existing systems.
Skilled workforce shortages, maintaining clinical standards outside the hospital and coordination across distributed teams are some of the issues.
Homecare requires nurses, therapists, and clinicians who can work autonomously in unpredictable environments. There is a shortage of nurses and therapists experienced in managing complex cases in home settings.
Deepak Sharma, CEO, MedLern highlights that, “The biggest challenge hospitals face is equipping staff to deliver care independently in unpredictable home environments. Unlike controlled hospital settings, homecare requires strong clinical judgement, autonomy, and adaptability skills that need specific training for nurses or allied professionals.”
Dr Gupta outlines the difficulty of maintaining consistent clinical standards in varied home environments, from infection control to documentation.
Dr Gaekwad adds that, “To ensure safety and quality, hospitals need standardised protocols that guide assessment, triage, and escalation. Comprehensive admission criteria help determine which patients are appropriate for home care based on clinical stability, home environment suitability, and caregiver availability. Evidence-based care pathways ensure consistency across clinicians and patient populations.”
Lathwal echoes this, noting that homecare “demands better operational planning than a hospital,” including SOPs, credentialed providers, 24/7 command centres, integrated EMR systems and quality monitoring programs.
Homecare also depends on seamless communication between hospital units, homecare teams, specialists, and digital platforms. Any gap can lead to delays, errors or safety risks—making communication infrastructure vital.
What’s holding home healthcare back?
Despite clear advantages, adoption in India remains uneven. Experts highlight four friction points:
◆ Clinical: Hospitals hesitate due to concerns about monitoring, emergencies and variation in quality
◆ Logistical: Coordinating staff, medical equipment and travel across large geographies remains complex especially outside major metros
◆ Financial: Less than 10 per cent of private insurance plans reimburse structured homecare. Out-of-pocket costs deter many families
◆ Technological: Fragmented platforms, low interoperability, patchy connectivity and varied digital literacy slow scaling.
Technology as an enabler
Whether it’s Tier 1 cities or remote districts, experts agree that technology is the force making homecare reliable and scalable.
Remote monitoring devices track vitals such as BP, ECG, SpO2 and glucose in real time.
Teleconsultations enable specialist oversight regardless of distance. Portable diagnostics bring X-rays, ECGs and blood tests to the patient’s doorstep.
Lathwal highlights that “Automation of alerts and clinical dashboards help in early detection of complications and improved emergency response.”
Dr Beri calls Remote patient monitoring (RPM) “transformative,” noting that it reduces ED visits and admissions significantly.
But technology alone is not enough.
Sharma says, “Technology adoption also varies, particularly when staff are unfamiliar with using remote monitoring tools or digital documentation systems.”
Tier 2 & Tier 3 India: Where homecare becomes a healthcare equaliser
While metro cities are driving early adoption, the greatest long-term impact of homecare will likely be felt in Tier 2 and Tier 3 regions.
Dr Gupta explains, “Home healthcare integrated with teleconsultation can greatly improve access to care in Tier2 and Tier-3 regions by reducing the need for patients to travel to larger cities. Teleconsultation enables early triage, specialist follow-ups, chronic disease management, and oncology reviews while homebased diagnostics (ECG, blood tests, dressings, IV therapy) are supervised remotely.”
Healing, comfort, and family support
Home-based care improves the patient experience in ways hospitals cannot replicate.
“Care which is provided in familiar surroundings helps to reduce the level of anxiety, enhances comfort, and encourage the participation from family as well. Medication and therapy adherence can also be improved by daily oversight. Acceptance of the same has grown very significantly especially after the covid as the family values care that avoid frequent visit to hospital”, says Dr Shetty.
Patients sleep better, adhere more consistently to treatments, and experience lower stress.Family involvement naturally increases enhancing emotional support and improving health literacy.
The strategic advantage: A new growth engine for hospitals
For hospitals, homecare is not merely a service line but a strategic necessity.
Hospitals can expand into chronic care packages, stepdown ICU, oncology aftercare, palliative care, home dialysis, rehab programs and home diagnostics. Moving stable patients home frees up beds, reduces ALOS, and increases ICU availability.
Homecare strengthens long-term patient relationships. As Dr Beri says, “When people feel cared for throughout their recovery, they tend to trust their healthcare partners more and stay with them longer.”
The warning and the opportunity
Dr Ravi Pratap, Consultant and Head of Emergency Medicine, Jupiter Hospital Pune points out that hospitals ignored homecare for years, allowing unorganised players to mushroom. He believes hospitals must reclaim the space by building dedicated teams, integrating insurance, and using their brand credibility and clinical depth to organise this fragmented sector.
His reminder is timely: “When the winds of change blow, some build walls and others build windmills.”
Way forward
Homecare is no longer an optional service. It is the next chapter in India’s healthcare evolution-one built on convenience, digital integration, and patient empowerment.
Hospitals that embrace homecare today will define the healthcare landscape of tomorrow.
[email protected]
[email protected]
- Advertisement -


