Gut health is most ignored in senior care and the most consequential
Ishaan Khanna, CEO, Antara Assisted Care Services highlights that age-related changes in gut motility, enzyme production and microbiome diversity directly impair nutrient absorption, immune function and medication tolerance in older adults, making gut health a foundational determinant of recovery capacity and overall well-being. This is not a niche issue. It is a care-design gap with cascading clinical, operational, and economic consequences
As India’s senior population grows, healthcare systems are preparing for more chronic diseases, longer lifespans, and rising care complexity. Yet one of the most consequential drivers of outcomes in older adults remains structurally under-addressed: Gut health. This blind spot is not marginal.
Studies show that 40 per cent of all elderly patients in India suffer from gut-related problems. Chronic constipation, Irritable Bowel Syndrome (IBS) and Irritable Bowel Disease (IBD), all of which severely impact daily life and health, are among the most reported conditions among the elderly in India with prevalence of 22 per cent, 5.4 per cent and 4 per cent, respectively.
Age-related changes in gut motility, enzyme production and microbiome diversity directly impair nutrient absorption, immune function and medication tolerance in older adults, making gut health a foundational determinant of recovery capacity and overall well-being.
This is not a niche issue. It is a care-design gap with cascading clinical, operational, and economic consequences.
Ageing gut is clinically different
In younger adults, gut disruption is uncomfortable; in seniors, it is destabilising. Ageing alters the gut in fundamental ways, slowing digestion, weakening the gut barrier, and reducing microbial diversity, with changes starting around midlife. Yet in practice, seniors presenting with fatigue, weakness, or recurrent infections often undergo extensive diagnostics, while underlying malabsorption or dysbiosis go unaddressed. Polypharmacy worsens gut microbiome imbalance, which in turn reduces medication effectiveness and tolerance.
Nutrition, hydration, and physical activity remain foundational to gut health at any age. However, in older adults, digestive capacity and nutrient absorption change significantly. Many seniors consume nutritionally adequate diets yet remain functionally deficient. This gap between intake and absorption explains why diet and lifestyle interventions alone often fail to deliver sustained improvement in gut-related outcomes among the elderly.
Clinicians consistently observe that gut dysfunction in older adults triggers systemic effects, amplifies frailty, reduces resilience, increases infection risk, worsens glycaemic control, delays post-illness recovery, and even spirals into hospital admissions. Interviews with doctors indicate that nearly 30 per cent of elderly patients presenting with gastrointestinal issues eventually require hospitalisation, particularly when these conditions are compounded by diabetes, hypertension, or cardiac disease. The result is a silent inflation of healthcare utilisation not driven by acute disease, but by physiological fragility.
The hidden cost
For providers and caregivers, this translates into higher readmission risk, longer recovery t imelines, increased caregiver dependency, poorer quality of life even when clinical parameters look stable. In India, out-of-pocket expenditure still accounts for around 39–40 per cent of total health expenditure, making preventable gut-related admissions particularly costly for families while pressuring already burdened health systems.
Yet in most care pathways, the gut is addressed reactively, after symptoms escalate, and not proactively as a determinant of resilience. This gap leads to late intervention and generic solutions. By the time clinical care is sought, decline has often progressed, narrowing the window for preventive intervention. This happens despite geriatric medicine being multi-disciplinary at its very core.
Why current senior care models fall short
Unlike organ-specific conditions such as heart or kidney disease, gut dysfunction touches almost every domain of senior health at once—from nutrient absorption and medication response to immunity, cognition, and mobility—making it one of the most consequential yet least systematically addressed systems in ageing care.
Growing clinical evidence links chronic gut dysbiosis to systemic inflammation (inflammaging) and disruption of the gut-brain axis with knock-on effects on cognition and mood in older adults. These pathways are increasingly being explored in relation to neurodegenerative diseases such as Alzheimer’s and Parkinson’s, and while much of this work is still emerging, it reinforces that gut health is not just about digestion but about brain and functional ageing.
What needs to change
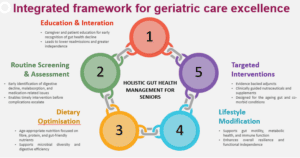
If senior care is to move from the existing model of reactive, episodic care to being proactive and preventive, gut health must be embedded into routine care design. The first conclusive step towards addressing this gap holistically can be making gut health assessment a baseline geriatric health metric alongside mobility, cognition, and vitals.
Clinically, it has been observed that many seniors cannot achieve adequate symptom control or nutrient absorption through lifestyle and diet changes alone, especially in the presence of multiple chronic conditions and polypharmacy. Here, evidence-backed nutraceuticals designed specifically for the ageing gut can play a critical role, not as a standalone cure, but as part of a continuous preventive care plan. When clinically guided, such interventions can help stabilise gut function while reducing pill burden, symptom severity, and supporting recovery, thereby lowering the risk of complications that often push seniors toward acute care. This approach carries clear economic relevance in India, where out-of-pocket expenditure still accounts for 39.4 per cent of total health expenditures.
Equally important is educating caregivers and clinicians—and seniors themselves—to recognise symptoms of early gut decline, such as persistent constipation, unexplained fatigue, bloating even after small meals, recurrent infections, and weight loss; healthy guts show regular bowel movements, stable energy, and fewer illnesses.
Holistic gut health management must also be integrated into recovery and chronic disease pathways, where it directly influences resilience and recovery speed. This is not about adding another supplement to the regimen; it is about building physiological stability into the way ageing care is delivered.
India is entering a phase where longer life spans without physiological resilience will overwhelm families and systems. Gut health sits at the centre of this equation, influencing how quickly seniors decline, how often they are hospitalised, and how hard recovery becomes.
- Advertisement -


