HAIs in CCUs: An overlooked burden
HAIs are a silent threat in India’s CCUs, where fragile patients face life-or-death stakes. Preventable yet persistent, these infections undermine the progress of advanced heart care. Can India make cardiac healing truly safe?
 Hospital Acquired Infections (HAIs) have long been recognised as one of the concern in modern healthcare. These infections are seen across multiple hospital settings, but their impact is particularly devastating in Cardiac Care Units (CCUs).
Hospital Acquired Infections (HAIs) have long been recognised as one of the concern in modern healthcare. These infections are seen across multiple hospital settings, but their impact is particularly devastating in Cardiac Care Units (CCUs).
Cardiovascular disease is the leading cause of death in India. With rise in demand for advanced cardiac care, tackling HAIs in cardiac units has become a matter of urgency.
Burden of HAIs in India: Scale of the problem
CCU patients are already fragile, recovering from major surgeries or on invasive devices. For them, an infection is not just an added complication but can be life-threatening. Infections such as ventilator-associated pneumonia (VAP), central line–associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), and surgical site infections (SSI) prolong hospital stays, escalate treatment costs, and significantly increase the risk of mortality.
Dr Anil Kumar, HOD and Senior Consultant-Medical ICU, Sharda Care Healthcity, explains that, cardiac surgery ICUs (post-cardiac surgery units) differ from medical CCUs in their HAI profile because patients are highly invasive-device dependent in the immediate post-op period.
He also mentions, “Indian studies show 4–10 per cent incidence of HAIs after cardiac surgery, higher than medical CCUs (~1 per cent). Device-associated infections remain the main contributors because nearly all patients require mechanical ventilation, central venous lines, arterial lines, urinary catheters, and pacing wires. Mortality and morbidity are significantly increased when HAI occurs in post-cardiac surgery patients, especially due to mediastinitis and bloodstream infections.”
Dr Nitin Prasar, Cardiologist, Silverstreak Multispeciality Hospital said, “HAIs in cardiac care units are around 1–4 per cent. They are predominantly device-associated HAIs: Ventilator-Associated Pneumonia (VAP), Central Line–Associated Bloodstream Infection (CLABSI), and Catheter-Associated Urinary Tract Infection (CAUTI). Indian ICU surveillance typically finds pooled rates around: VAP ~9–13, CLABSI ~5–11, CAUTI ~2–7 per 1,000 device-days (ranges vary by hospital and year).”
Dr Ranjan Modi, Senior Consultant & Head – Interventional Cardiology, Sarvodaya Hospital notes, “In high-acuity cardiac units, device use is intense, so our infection profile skews toward device-associated events. Across Indian ICUs, multiple surveillance efforts have shown double-digit rates per 1,000 device-days for ventilators, central lines, and urinary catheters; cardiac ICUs generally mirror this risk because of post-operative ventilation, multiple lines, and longer stays.”
“In our practice, ventilator-associated pneumonia (VAP) and central line–associated bloodstream infection (CLABSI) lead the tally, with catheter-associated UTI (CAUTI) close behind. Poststernotomy surgical-site infections are less frequent but particularly consequential, and deep sternal wound infection/mediastinitis, though uncommon, carries high morbidity. The microbial landscape is dominated by multidrug-resistant gram-negatives—Acinetobacter, Klebsiella, Pseudomonas—alongside MRSA. The takeaway is simple: the burden is real, but it is predictable and preventable when we standardise bundles, measure consistently, and act on our own data.”
 Cardiac patients especially vulnerable: Why?
Cardiac patients especially vulnerable: Why?
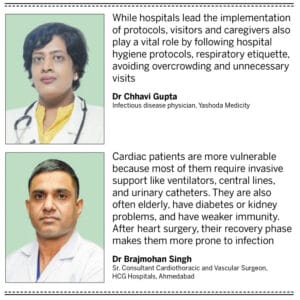
Infections in CCUs are majorly the outcome of various risk factors like combination of clinical vulnerability, spme invasive procedures and other comorbities such as diabetes, obesity or kidney diseases. Dr Chhavi Gupta, Infectious disease physician, Yashoda Medicity stresses, “Cardiovascular diseases are predominantly seen in the elderly population and individuals with chronic conditions such as diabetes and hypertension. These comorbidities, coupled with advancing age, contribute to a weakened immune system, making cardiac patients highly susceptible to a broad range of infections— especially HAIs. In India, HAIs remain a persistent concern in CCUs. Studies indicate HAI incidence in Indian CCUs ranges from 15 per cent to 25 per cent, significantly higher than the global average.”
Dr Brajmohan Singh, Sr. Consultant Cardiothoracic and Vascular Surgeon, HCG Hospitals, Ahmedabad explains, “Cardiac patients are more vulnerable because most of them require invasive support like ventilators, central lines, and urinary catheters. They are also often elderly, have diabetes or kidney problems, and have weaker immunity. After heart surgery, their recovery phase makes them more prone to infection.”
Infection Control and Prevention (IPC): What matters the most?
Experts agree that these infections are largely preventable with the right protocols, technologies, and systemic reforms. Dr Neeta Shrivastava, Consultant Microbiology and Head Infection Control, Medicover Hospitals, Navi Mumbai highlights, “Strict adherence to sterile techniques during surgery and device insertion, along with timely removal of invasive lines, will help to reduce HAIs. Consistent hand hygiene, antibiotic stewardship, and dedicated infection surveillance are important for cardiac patients.”
Dr Singh also shares that, “Simple, consistent practices give the best results – like proper hand hygiene, strict care bundles for ventilators and central lines, timely removal of unnecessary catheters, and correct antibiotic use. For surgical patients, maintaining blood sugar control, proper skin preparation, and using antibiotics at the right time before surgery are extremely important.”
Dr Kumar cites that device specific bundles are another successful method of IPC. A CLABSI prevention bundle for example includes certain steps taken by the staff (such as using a checklist to insert lines, daily assessment of the need for the line, and ensuring skin preparation includes the use of chlorhexidine). A VAP bundle would include ensuring the head of the bed is elevated, encouraging daily breaks from sedation, and oral care with chlorhexidine.
Dr Gupta believes that infection prevention is a shared responsibility. She mentions, “While hospitals lead the implementation of protocols, visitors and caregivers also play a vital role by following hospital hygiene protocols, respiratory etiquette, avoiding overcrowding and unnecessary visits, especially during outbreak situations.”
This underlines a critical insights-preventing HAIs is more about relentless execution of basic hygiene and care protocols.
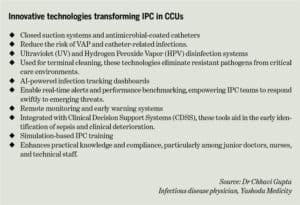
Dr Swarup Swaraj Pal, Chief CVTS surgeon, Cardiovascular and Thoracic, MICS, Trauma and Transplant surgeon, Gleneagles Hospital cites, “In CCUs, innovations like antimicrobial-impregnated lines, automated hand hygiene monitoring, and AI-driven infection tracking systems are helping reduce HAIs.”
Dr Kumar believes that innovative developments in preventing healthcare-associated infections (HAIs) are moving away from using tried-and-true measures. One promising avenue of HAI prevention is the use of automated disinfection technologies, e.g., ultraviolet light (UV-C) devices and hydrogen peroxide vapor systems, which are employed in patient rooms after a patient is discharged, to supplement the manual cleanliness of the room. These automated disinfection devices are an effective way to decontaminate surfaces and decrease resilient pathogens such as Clostridium difficile or Methicillin-resistant Staphylococcus aureus (MRSA).
Dr Surya Prakash. S, Senior Consultant, SRM Global Hospitals, Chennai mentions, “AI-powered infection monitoring systems, UV-C light cleaning equipment, and catheters coated with antimicrobials are now all used simultaneously in certain cardiac intensive care units. Rapid pathogen detection kits make it simpler to identify and treat illnesses early on.”
“Certain hospitals have also incorporated robotic disinfecting systems to provide thorough surface sterilisation of important areas. Wearable biosensors are also in the pipeline to constantly monitor patients’ vital signs and identify initial indicators of infection. Telemetrylinked infection alerting enables clinicians to act in real time, while antimicrobial dressing for surgical wounds of high technological value continues to minimise infection incidence in post-cardiac surgery patients.”
Rapid diagnostic kits and molecular testing are another area of promise, as they allow clinicians to identify pathogens and resistance patterns within hours instead of days, reducing delays in targeted therapy.
However, as several experts pointed out, these innovations are resource-intensive and not yet widely accessible across India. “The challenge is that these tools are expensive, so not everyone can use them,” admits Dr Manoj, Consultant Intensivist, VS Hospitals, Chennai.
Operational and systemic barriers
If prevention is straightforward and technologies are advancing, why do HAIs remain such a persistent problem? The answer lies in operational and systemic challenges.
“The challenges are mainly operational. In busy ICUs, following every step of the infection-prevention protocol is difficult, especially when patient load is high. Staffing shortages, frequent turnover of nurses and technicians, and limited availability of advanced equipment also make it harder. Antimicrobial resistance is another growing problem.” says Dr Singh.
Dr Manoj echoes this, highlighting that, “We don’t have enough nurses for the number of patients we admit. Even the best infection-control plans falter when each nurse is stretched too thin. Infrastructure doesn’t always help; many ICUs still don’t have enough isolation rooms or even enough hand-rub bottles at the bedside. High patient turnover, constant crowding, and resistance to changing old habits make it worse. And in resource-limited hospitals, infection prevention often loses out to more immediate needs like beds and ventilators.” Resource-limited hospitals often face additional issues: overcrowding, outdated infrastructure, inconsistent sterilisation, and limited diagnostic facilities. Moreover, antimicrobial resistance (AMR) compounds the challenge, narrowing treatment options and driving up costs.
 Regulatory and policy changes
Regulatory and policy changes
Experts agree that we need stronger national level policy ecosystem to tackle HAIs in CCUs. Currently, reporting is patchy, protocols are inconsistent, and accountability is weak.
Dr Singh said, “We need standard guidelines for all hospitals to monitor and report infections in the same way. Dedicated infection-control teams should be mandatory, with proper staff and training. Hospitals should also be encouraged to follow antibiotic stewardship programs, so that antibiotics are used wisely.”
Dr Shrivastava also mentions, “Standardised IPC protocols, backed by audits and accountability measures, would help ensure consistent infection control across hospitals.”
Dr Modi calls for universal, comparable HAI surveillance across cardiac units — both public and private — tied to national accreditation standards. “None of this requires cutting-edge tech; it requires standards, transparency, and steady resourcing so that the best practices in a few centres become the norm everywhere,” he says.
Experts also advocate for mandatory HAI reporting, dedicated infection-control professionals, multilevel audits, and protected funding for IPC infrastructure and staff training.
Dr Prakash said, “In addition, establishing dedicated infection control units within every cardiac hospital, incentivising compliance through accreditation programs, and integrating AI-driven surveillance into national health databases could further enhance prevention. Public awareness campaigns about hospital-acquired infection risks and the importance of early reporting can also support safer cardiac care environments.”
Way forward
HAIs are a silent threat in India’s CCUs, where fragile patients face life-or-death stakes. Preventable yet persistent, these infections undermine the progress of advanced heart care. Can India make cardiac healing truly safe?
Dr Manoj said, “Every day in the CCU, we see patients and families put their trust in us at their most vulnerable moment. They come to us hoping for a second chance at life. The least we owe them is care that is not only advanced but also safe from preventable infections”.
Proper execution of basic IPC measures, scaling up the adoption of technology, stronger policy frameworks, and adequate staffing and training is the need of the hour. Infection control in hospital should not be seen as an addon, but as integral part of the cardiac care ecosystem.
- Advertisement -